The Metabo-oncology Company
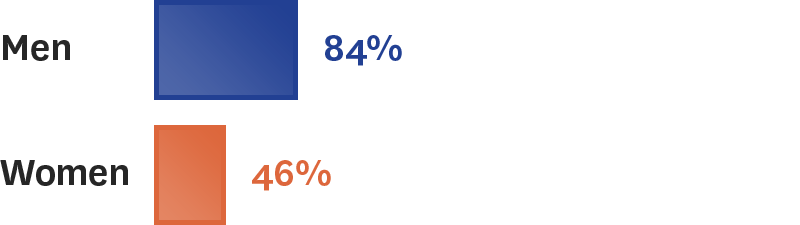
Metabo-oncology — the overlap of obesity + cancer — is the next wave in cancer patient treatment.
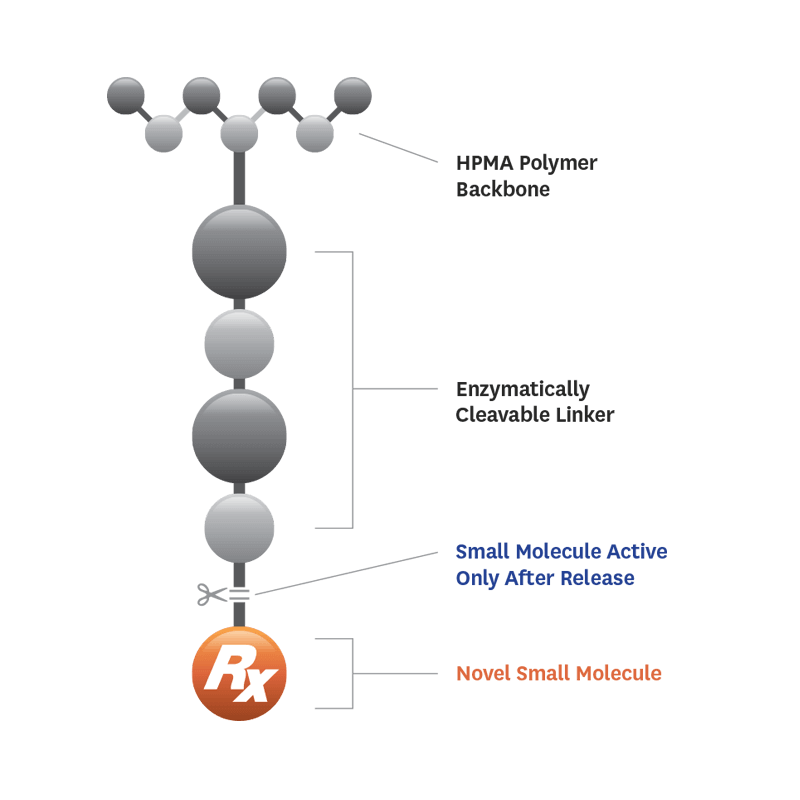
Cancer cells co-opt metabolic hormones (e.g., insulin, leptin) to proliferate, resulting in cancer progression and metastases. Yet, the many cancer patients also have insulin resistance. This metabolic state affects millions of cancer patients worldwide is overlooked as a major contributor to cancer progression. What’s worse, many anti-cancer treatments cause metabolic dysfunction, limiting treatment effectiveness and even leading to treatment resistance.
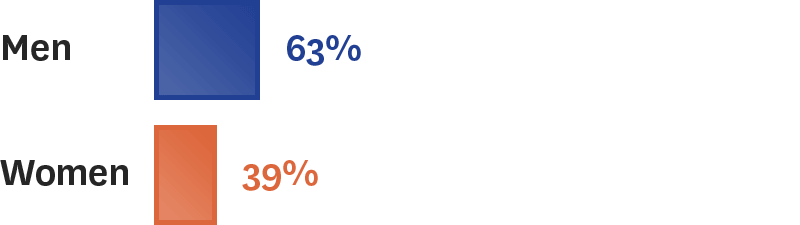
SynDevRx – the leader in the emerging field of metabo-oncology – is tackling this urgent and unmet medical need with its clinical drug evexomostat (SDX-7320).